Assess
Comprehensive preparation before the first word.
-
Psychiatric intake or psychological testing—your preference
- Supports documentation for evaluations, testing, health behavior, and cognitive assessments
- Team members can help with intake prep; clinicians focus on interpretation and treatment decisions
What changes when you use Assess
Without Assess
Intake data scattered across EMRs, paper forms, and your memory
First visit eaten by fact-finding instead of formulation and treatment
Important details and patterns discovered late, if at all
Billing notes written from scratch under time pressure
Depression that doesn’t respond. Another medication trial. The pattern stays invisible.
With Assess
First visit focused on making sense of the case and deciding what to do
Risks, patterns, root causes, and social determinants surfaced before you walk in—so you can practice true biopsychosocial medicine
Clinical documentation ready for the evaluation or testing you’re actually doing
Assessment revealed “good symptom days” were actually hypomania. Treatment shifted from antidepressants to mood stabilizers. Diagnosis: Bipolar II—preventing potential mania trigger.*
* This case is from our partnership with Texas Center for Lifestyle Medicine. Patient details anonymized.
Whole-person assessment, one workflow
What Assess actually catches
These findings come from real assessments during clinical validation. They’re easy to miss in 15-minute visits—and expensive to miss long-term.
These aren’t edge cases. They’re what comprehensive assessment finds when you look deeply enough.
Catch 1 — The Supplement Paradox
Found: Patient taking daily ashwagandha for brain fog—a supplement with documented brain fog as a side effect.
Why it matters: The treatment was perpetuating the problem. Stopping the supplement was the intervention, not adding medication.
Missed because: Supplement reconciliation rarely goes beyond “do you take vitamins?” Ashwagandha is generally considered benign.
Catch 2 — Bipolar Hidden in "Good Days"
Found: Positive mood disorder screening that patient dismissed as “just feeling better for once.” Detailed history revealed decreased sleep need, rapid speech, increased activity, reckless spending.
Why it matters: Diagnosis changed from Major Depressive Disorder to Bipolar II—fundamentally altering treatment. Antidepressants alone could have triggered mania.
Missed because: Patients normalize hypomania as relief from depression. Brief screening doesn’t capture “tell me about a time you felt really good.”
Catch 3 — The Anxiety That Was Loneliness
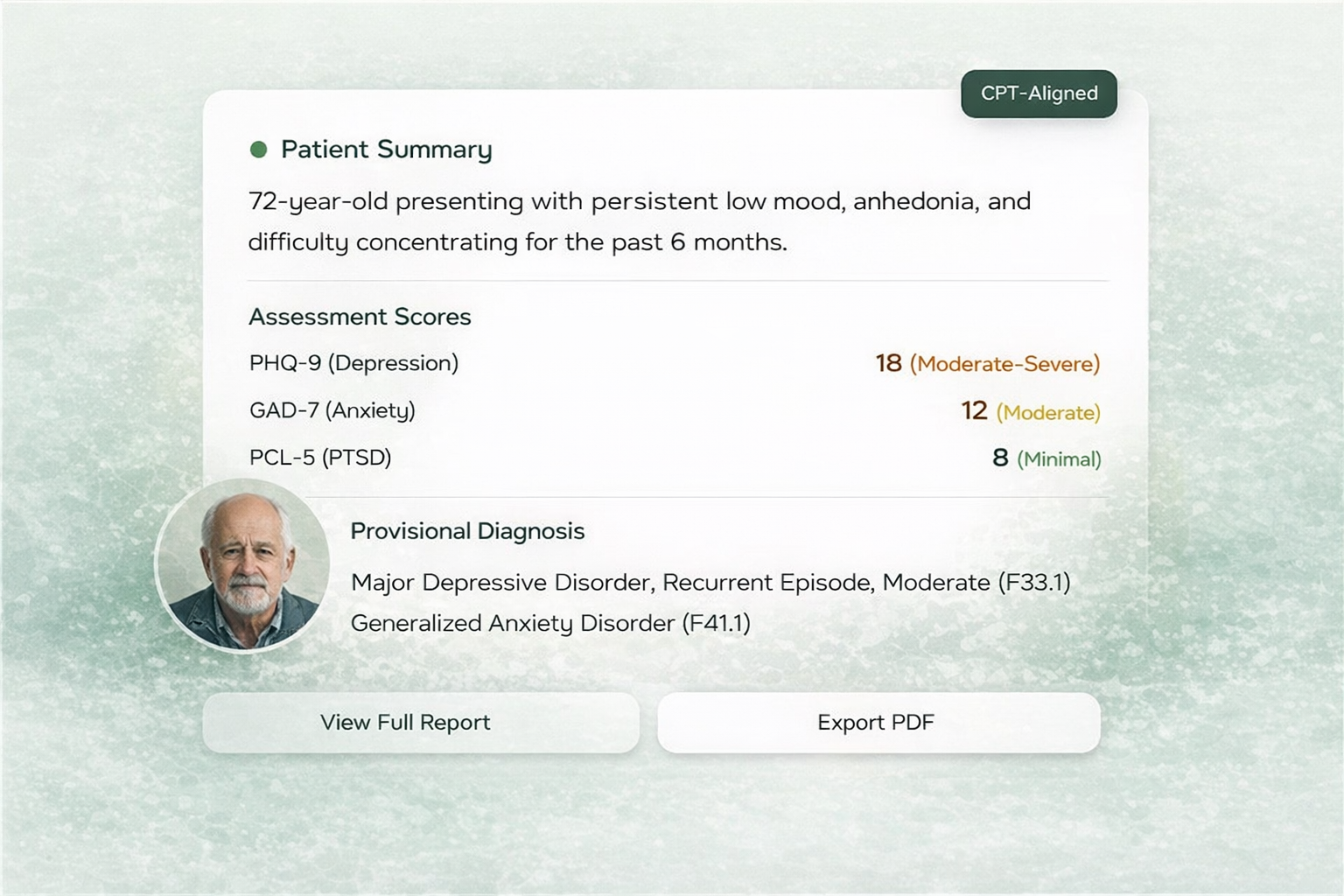
Found: 72-year-old convinced he had early dementia. Cognitive testing normal. Detailed social assessment revealed he lived alone on rural property, nearest family 1,500 miles away, no one to drive him home from medical procedures.
Why it matters: His “memory problems” were attention deficits from chronic anxiety. His “lack of motivation” was avoidance from overwhelm. Treatment: community connection, not dementia workup.
Missed because: Standard psychiatric care focuses on symptoms and medications, rarely assessing practical social support infrastructure.
Catch 4 — Caffeine Self-Medication
Found: Six espresso shots daily in a patient referred for social anxiety. Patient knew “this may be a problem” but no one had quantified it or connected it to her symptoms.
Why it matters: She was self-medicating probable ADHD with caffeine, which was then amplifying her anxiety. The fix wasn’t an SSRI—it was reducing caffeine, then evaluating for ADHD.
Missed because: Standard intake asks “do you drink coffee?” not “how many shots?” Caffeine is rarely assessed as a primary driver.
Catch 5 — The MDQ Artifact
Found: Positive bipolar screening (10/13 items) in a 37-year-old veteran. But exploration revealed all symptoms occurred 7+ years ago during active alcoholism—none currently.
Why it matters: Prevented inappropriate bipolar diagnosis and mood stabilizer prescription in a patient who had been successfully medication-free for seven years.
Missed because: Screening tools don’t capture temporal context. A positive MDQ typically triggers mood stabilizer discussion without asking “when did this happen?”
Psychiatric Intake or Psychological Testing — your choice
Comprehensive diagnostic evaluations
- 90792 — Psychiatric diagnostic evaluation
- 99205/99215 — High-complexity E/M, when medical evaluation is primary
- 96156+ — Health behavior assessment & intervention, when appropriate
- 99483 — Cognitive assessment & care plan, when indicated
Psychological testing workflows
- 96136–39 — Technician-administered testing
- 96130–31 — Psychological testing evaluation by QHP
- 96127 — Brief emotional/behavioral assessment, when useful
Who uses Assess
Built for behavioral health and primary care practices that want to deliver excellent care sustainably.
Assess is already working in real clinics

10 years in my own psychiatry practice
“Assess is the embodiment of workflows I’ve run in my San Francisco practice for a decade: structured whole-person intake, embedded measurement, and clear documentation for evaluations and testing.
Roughly 400 patients have gone through this approach. It’s how I practice psychiatry every week.”
— Ravi Hariprasad, MD, MPH
Clinical validation in integrated primary care
We validated Assess at Texas Center for Lifestyle Medicine, an integrated primary care clinic in Houston. Patients with combined mental and physical health challenges received comprehensive AI-assisted assessments as part of their Assessment Clinic.
”"This challenged my belief system—that the only way you can really identify mental health challenges was with a qualified mental health practitioner. But that's not what we found whatsoever."
— Dr. Cheng Ruan, MDFounder, Texas Center for Lifestyle Medicine
*Note: This pilot focused on the Assess/myJourney layer; Monitor and Care were not part of this phase. A more detailed case study is available for interested partners.

What we found:
-
45 patients completed comprehensive assessments
-
Condition distribution: 33% depressive disorders, 27% anxiety disorders, 9% PTSD, 7% mild cognitive impairment
-
Average of 8–10 clinically relevant conditions surfaced per patient versus literature benchmark of 2.8
-
Root causes identified: sleep disruption, caffeine patterns, supplement interactions, undisclosed trauma
What clinicians experienced:
-
Less time reconstructing patient histories
-
More time for formulation and treatment planning
-
Comprehensive behavioral evaluations inside primary care—no specialty referral needed
What clinicians and patients notice
What clinicians experienced
- Walking into first visits with a structured understanding—not starting from zero
- Less repetitive questioning—the assessment captured it, patient confirmed
- Clearer identification of contextual drivers: social isolation, sleep, substance use, relationships, financial stress
- Findings that change care plans, not just confirm them
“The detailed assessment let me spend more time with patients discussing recommendations. Organizing information beforehand made the consult more efficient and productive.”
— Therapist, Texas Center for Lifestyle Medicine
What patients experienced
- Feeling that the assessment “asked the right things”—not just symptom checklists, but context about sleep, relationships, substances, and daily life
- Greater understanding of how different areas of their lives fit together
- For some, addressing upstream factors led to meaningful improvement within weeks
- Frequently noting that no prior clinician had connected all the pieces
“It was the first time I felt like the whole picture of my life was being considered, not just my symptoms.”
— Patient, age 72
Complete on its own. Ready to grow with you.
Common questions about Assess
How do I know Assess actually works?
In our clinical partnership with Texas Center for Lifestyle Medicine, Assess identified an average of 8-10 diagnoses per patient versus the literature benchmark of 2.8. Assessment surfaced findings standard care would have missed: bipolar disorder masked as treatment-resistant depression, supplements causing the symptoms they were meant to treat, profound social isolation driving anxiety symptoms, and undisclosed trauma affecting daily functioning.
These weren’t edge cases—they were typical patients referred from primary care. We have detailed case documentation available for practices considering Assess.
Do we have to redo all our intakes?
No. We start by mapping Assess to your current evaluation practices. Many clinics adopt it as a structured backbone and then refine over time.
Can non-clinicians help patients complete the assessment?
Yes. Many teams have care coordinators, technicians, or support staff assist patients. Licensed clinicians always retain final responsibility for interpretation and clinical decisions.
Do we need to switch our EHR?
No. You can run Assess alongside your current EHR and export summaries. Where integration is available, we can post key artifacts back with provenance.
Does Assess make diagnoses or treatment recommendations?
No. Assess is a documentation and workflow tool that organizes information and surfaces patterns. It supports clinician judgment; it does not make diagnoses or prescribe treatment.
How do you handle privacy and HIPAA?
Will this work for our specific payers and state rules?
We’ll look at your panel, payers, and state requirements during a practice assessment. We don’t guarantee reimbursement; we help you document cleanly and choose service lines that are realistic for your environment.
Can we see real examples of outputs?
Yes. We can share de-identified, watermarked samples (clinician summary, PCP summary, patient handout, billing note) after a brief conversation.
Can we use Assess without Monitor and Care?
Yes. Many practices use Assess as a standalone solution and find it delivers complete value on its own — deeper first visits, cleaner documentation, findings that standard intake misses. Monitor and Care are optional extensions for practices ready to add routine measurement and care coordination. You decide what makes sense for your situation.
How long does a typical assessment take?
The full assessment process involves about 30 minutes of patient self-report (completed on their own time), followed by a 30-minute call with your care coordinator, health coach, or clinician to close gaps and confirm key items. Then your standard intake visit proceeds as usual — but now you walk in with a complete clinical picture already organized. The outcome is a level of insight that would normally take multiple visits to develop, and it’s billable against psychological testing codes for additional revenue.
What happens if a patient can't complete the assessment before their appointment?
Assess is flexible. Patients can complete the self-report portion in your waiting room, or your team can conduct a brief verbal intake using the same framework. The assessment can also be split across multiple touchpoints if needed. The goal is a complete picture, however you get there.
Can we customize which domains are included in the assessment?
Our flagship myJourney assessment covers comprehensive domains and is included with Assess. Custom assessments can be designed based on your specific evaluation needs — for example, emergency room evaluations, pain management clearances, surgical clearances, or specialty-specific intakes. Contact us for a quote on custom assessment design.
How does Assess handle patients with low literacy or language barriers?
The assessment uses plain language designed for accessibility. For patients who need additional support, staff can assist with completion verbally. We’re actively expanding language support — let us know your specific needs and we’ll discuss options.
Ready to see what Assess would look like in your clinic?
Assess is more than a better form—it's a different starting point for care.
If you want to understand how it could fit with your clinicians, workflows, and payers, the best next step is a practice assessment.
Ready to talk? Get a practice checkup.
Want to stay informed? Join the Assess waitlist.

